Arrhythmia
Arrhythmia is often suspected when symptoms of palpitation, dizzy spells or syncope are present but can be found incidentally during a routine pulse check by your own doctor. There are several different types of arrhythmia or channelopathies which may cause such symptoms including the following:
- Sinus node dysfunction
- Atrioventricular block
- Supraventricular tachycardia (SVT)
- Ventricular tachycardia (VT)
- Ventricular fibrillation (VF)
- Atrial fibrillation (AF)
- Atrial Flutter
- Atrial tachycardia
- Premature atrial or ventricular ectopics
- Bundle branch block
- Inherited or congenital long QT syndrome
- Brugada syndrome
The specific arrhythmic diagnosis requires confirmation, either by 12-lead ECG or continuous Holter ECG monitoring, followed by specialist evaluation. Patients often require a series of blood tests, an echocardiogram to assess for structural abnormalities of the heart, and sometimes an invasive electrophysiological study.
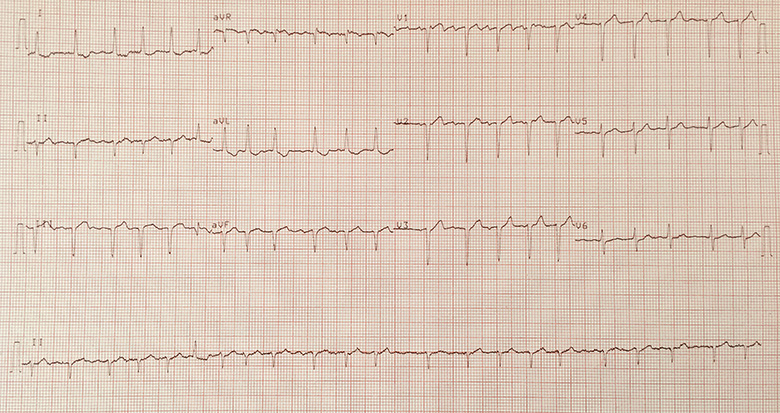
12-lead ECG demonstrating atrial fibrillation
Treatment options will depend on the specific diagnosis. This may consist of simple lifestyle measures alone however certain patients may require prescribed medication including heart rate controlling drugs or anti-arrhythmic drug therapy. Blood thinners called anticoagulants, such as warfarin or direct oral anticoagulants (DOAC), may be required for arrhythmia such as atrial fibrillation in order to reduce stroke risk. Selected patients may benefit from invasive procedures such as electrical cardioversion, catheter ablation procedures or pacemaker/defibrillator insertion.


